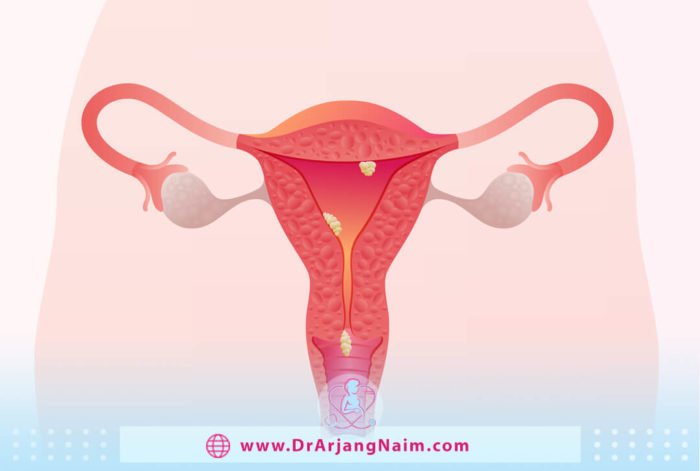
Uterine polyps are lesions that attach to the inner wall of the uterus and extend into the uterine cavity. Overgrowth of cells in the lining of the uterus leads to uterine polyps, also called endometrial polyps. These polyps are usually non-cancerous, although some of them can be cancerous or eventually turn into cancer.
The size of uterine polyps varies from a few millimeters (smaller than a sesame seed) to several centimeters (the size of a golf ball or larger). They attach to the uterus wall with a large base or a thin stalk. The uterus may have one or more polyps. They usually remain inside the uterus, but sometimes, they slip into the vagina through the cervix. Uterine polyps are more common in women going through menopause or who have completed it, although younger women can also get it.
Symptoms
When the symptoms of uterine polyps are apparent, it resembles the symptoms of more serious diseases, such as endometrial cancer. Symptoms may include a variety of abnormal uterine bleeding, such as:
- Heavy menstrual bleeding
- Spotting between periods
- Bleeding after intercourse
- Bleeding after menopause
Causes

The exact cause of the polyp is unknown. Maybe associated with changes in hormone levels. Each month, estrogen levels rise and fall, causing the uterus lining to thicken and then shed during menstruation. Polyps form when the lining grows too much.
Some factors may increase the risk of infection. One of these factors is aging. The risk of having polyps is higher in women 40 and 50 years old. This may be due to changes in estrogen levels that occur just before and during menopause. The following factors increase the risk:
- Obesity
- High blood pressure
- The breast cancer drug tamoxifen
Risk factors
Risk factors for uterine polyps include:
- Being perimenopausal or postmenopausal
- Having high blood pressure
- Being obese
- Taking tamoxifen, drug therapy for breast cancer
Uterine polyps and infertility

Infertility is defined as the inability to conceive after one year of trying. The prevalence of diagnosing suspected intrauterine abnormalities during hysteroscopy before in vitro fertilization was between 11% and 45%. Polyps can prevent the implantation of a fertilized egg in the uterus wall. They can also block the area where the fallopian tube connects to the uterine cavity and prevent sperm from moving into the tube to meet the egg.
Similarly, they can block the cervical canal, preventing sperm from entering the uterus. Polyps may also be involved in miscarriage in some people.
Diagnosis
There are several diagnostic methods that gynecologists examine.
Hysterosalpingogram (HSG)
Hysterosalpingogram (HSG) is a special x-ray of the uterus and fallopian tubes. HSG is performed after menstrual bleeding has stopped. This makes it easier to see the polyp and other tissues.
Ultrasound
Vaginal ultrasound is one of the most important and widely used tools in gynecology. In vaginal ultrasound, the body’s internal organs are evaluated using high-frequency sound waves.
Sonohysterogram
An ultrasound histogram is an imaging study of the uterus. The doctor injects saline (saline) into the uterus through the cervix to examine the uterine cavity. This method allows doctors to identify more structures than using ultrasound without fluid injection. This helps visualize polyps that may have been missed with traditional ultrasound.
Hysteroscopy
This procedure uses a scope inserted into the uterus through the vagina to look at the polyps and determine their size and extent. Part or all of the polyps can also be removed for microscopic examination by inserting a tool through a hysteroscopic tube.
Excision through traditional methods
A polyp sample may be obtained by curettage or biopsy or after a hysterectomy.
Examination of the tissue under a microscope is the only way to determine if the polyp is benign or malignant.
Treatment
Depending on the case, the doctor may recommend the following:
- Watchful waiting: If the person is asymptomatic and the polyp is not cancerous, treatment may not be needed, and it will go away on its own. If the person is at risk, the doctor decides to remove the polyp.
- Medications: Progestins and gonadotropin-releasing hormone agonists help control hormone levels. They may shrink polyps and reduce symptoms such as heavy bleeding. But the symptoms often return when the medication is stopped.
- Surgery: Doctors can usually remove polyps using the same methods to diagnose them, such as hysteroscopy or curettage. Instead of making an incision in the abdomen, they can insert a curette or other surgical instrument through the vagina and cervix to remove the polyps. If the polyps have cancer cells, surgery may be needed to remove the entire uterus, called a hysterectomy.
Uterine polyps vs. fibroids
Fibroids and polyps are similar, but there are a few differences. Uterine fibroids are overgrowth of the muscles inside the uterus walls, not the lining of the uterus. Fibroids, like polyps, can cause heavy bleeding and pain, constipation, and difficulty urinating.
Can uterine polyps be prevented?
There is no way to prevent uterine polyps. It is essential to have regular gynecological examinations. Risk factors such as obesity, high blood pressure, or taking tamoxifen to treat breast cancer may increase the chances of developing polyps. Sometimes uterine polyps come back after treatment, and additional treatment may be needed.
What is the natural treatment for polyps in the uterus?
To shrink cervical or endometrial polyps naturally, we need to look at all the factors that play a role.
Root cause
The dominance of estrogen causes polyps, in which case an imbalance is created between the levels of estrogen and progesterone, the two main female hormones. To correct this problem, estrogen overproduction can be reduced by changing the diet and supporting the normal production of progesterone. Under stress, ovulation may not occur. In this case, progesterone cannot be detected in a specific cycle. Stress management can help maintain progesterone.
Inflammation
There are a number of factors that irritate, aggravate, or cause inflammation in the body, including:
- Food sensitivities
- Insulin
- Poor diet
- Latent infection
- Chemicals
All of these factors are cured through natural remedies.
Low-grade food allergies cause inflammation in the body. This inflammation can be widespread and is not limited to the gut system. However, it can also present as digestive problems such as constipation, diarrhea, acid reflux, bloating, gas and nausea.
Insulin
Insulin is increased by consuming foods that raise blood sugar. It causes inflammation and abnormal tissue growth. Research shows an association between insulin resistance and endometrial polyps.
Latent infection
A latent infection is an infection that a person may not know. However, these low-grade infections can perpetuate cervical inflammation and contribute to polyps.
Poor diet

Some foods are anti-inflammatory, while others are inflammatory. For example, trans fats are more inflammatory. Some foods secrete much more insulin than others. An anti-inflammatory, low-carb diet can help.
Excessive estrogen production or activity
Carbohydrates and sugars in the diet increase blood insulin levels. Therefore, higher insulin increases estrogen production. Insulin also lowers sex hormone-binding globulin (SHBG) levels. SHBG helps control estrogen activity. Therefore, decreasing SHBG increases estrogen activity.
Excess estrogen
When the body has enough estrogen, the liver needs to process and break it down extra to remove it. Vitamin B6, Vitamin B12, Magnesium, 5 MTHF, Indole-3-carbinol, Sulfur, and Glucaric Acid. If the body does not have one or more of these substances, estrogen may not be completely converted to waste, so it is not completely excreted.
The bottom line
Uterine polyps form when cells grow abnormally in the inner wall of the uterus. Polyps are small, soft lumps inside the uterus that are usually 95% benign and treatable, although some can be cancerous or eventually turn into cancerous lumps. Most uterine polyps do not show any symptoms, and if they do, they show symptoms such as cancer of the uterus or endometrium. That is why it is necessary to see a gynecologist if you see such symptoms.
The possibility of polyps returning after treatment is rare, but it is necessary to treat it immediately if it occurs.
Dr. Arjang Naim, MD, chooses the best treatment for uterine polyps after a thorough examination of the client.
Additional questions
1. Do uterine polyps need to be removed?
Polyps should be treated if they cause heavy bleeding during menstruation or if they are suspected of being precancerous or cancerous. They should be removed if they develop problems during pregnancy, such as miscarriage or infertility in women who want to become pregnant.
2. How common are uterine polyps?
Uterine polyps are very common. 3 out of 10 women may get them at some point in their lives, but less than 1 in 100 women get polyps before 30. They usually occur before and after menopause.
3. Can the patient return to work after the removal of the uterine polyp?
Rapid recovery occurs after the removal of the polyp. After a polypectomy, patients can return to work the next day and expect a full recovery within two weeks.
4. What percent of uterine polyps are cancerous?
The risk of cancer in uterine polyps is low. In premenopausal women, this number is 1-2%. In women who have gone through menopause, the risk is 5-6%.
5. What is abnormal uterine bleeding (menometrorrhagia)?
Abnormal uterine bleeding is when you bleed between periods or when your period is very heavy or long.
References:
https://www.naturopathtoronto.ca/uterine-polyp/
https://www.mayoclinic.org/diseases-conditions/uterine-polyps/diagnosis-treatment/drc-20378713
https://my.clevelandclinic.org/health/diseases/14683-uterine-polyps
https://www.webmd.com/balance/take-stock-health-habits
https://www.verywellhealth.com/symptoms-of-uterine-polyps-3863207
https://www.columbiadoctors.org/treatments-conditions/uterine-polyps